Most diabetics accept the fact that the more carbohydrates (carbs) they consume the less stable, healthy, and consistent their blood sugars will likely become.
But why is that?
Is it only due to the sheer volume of carbs being consumed or are there other factors to consider?
Turns out it’s both!
Keep reading to find out what other factors carbs have that commonly influence unstable blood sugars.
What Many Diabetics Already Know About Carbs
There are only 3 macronutrients that exist in our diet:
- proteins
- fats
- carbs
The first macronutrient many people think about with any mention of “diabetes” is carbs.
The primary role of carbs is to be used or stored as energy (aka calories) in the form of glucose for the body.
Once energy demands are filled, the excess carbs are stored as fat. Normally in triglyceride form.
It’s common for diabetics to experience a wide variety of blood glucose levels while eating a carb-rich diet.
However, many diabetics attempt to continue eating as they did prior to their diagnosis and quickly realize thinking and functioning like their pancreas is not as easy as it may appear.
In other words, simply injecting “enough” insulin for the carbs consumed doesn’t normally work out that well or consistently.
The 4 dietary problems typically responsible for these unstable blood sugars are:
- The quality of carbs
- Miscalculated diabetic medication dosing
- Volatile blood glucose spikes and roller-coaster blood sugars
- Other dietary inflammatory factors
What Diabetics May Not Know About Carbs
Problem #1 – Carb Quality Matters
50 grams of sweet potatoes are not the same as 50 g of Oreo cookies.
Simply put, ultraprocessed foods are highly recommended to stay away from.
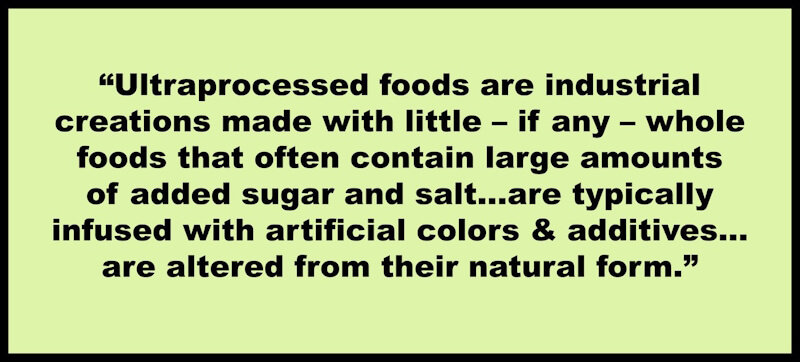
Quote Source: What Doctors Wish Patients Knew About Ultraprocessed Foods; https://www.ama-assn.org/delivering-care/public-health/what-doctors-wish-patients-knew-about-ultraprocessed-foods
Common ultra-processed foods, such as frozen pizza, cereals, fast food, canned soup, and most foods containing gluten (I call these foods glutenoids) have been linked to a dramatic increase in all-cause mortality by up to 62% among the general population (1).
Keep in mind, it doesn’t help that these nutrient-lacking Frankenfoods consist of approximately 57% of our daily calories consumed by American adults. Children are consuming an estimated 67% of daily calories from these ultraprocessed foods (2, 3)!
A couple of epidemiological studies even show a correlation of increased diabetes risk the more one consumes ultraprocessed foods (4, 5).
There was a recent argument made in the Harvard Public Health journal stating that processed foods are making everyone sick and that it’s time for the government to do a better job of stepping in to cushion this blow (6).
They base this notion on the fact that over 670,000 deaths per year are the result of ultraprocessed food consumption.
In addition, 2/3 of severe Covid-19 cases were attributed to four diet-caused diseases (7):
- Obesity
- Diabetes
- Hypertension
- Heart failure
There are other studies noting a higher risk for metabolic syndrome (common among diabetics), type 1, and type 2 diabetes development with higher processed food intake, as well (8, 9, 10).
Unsurprisingly, blood sugars appear to be consistently elevated among diabetics who have a higher intake of processed junk food, as well (11).
One of the most important symptoms of diabetes risk is sustained high blood sugar levels (aka hyperglycemia), which many of these carb-rich foods are typically known to contribute towards (12).
In addition, these high-caloric and low-nutrient foods don’t help support diabetic health the way many whole foods do. The reason why is that most whole foods have a much greater variety of vitamins and minerals than almost all ultraprocessed Frankenfoods.
For example, some important nutrients that normally assist with better blood sugar stability are:
- Chromium: shellfish, broccoli, grass-fed meats
- Alpha-lipoic acid: dark green vegetables, organ meats, red meat
- Magnesium: pumpkin seed kernels, dry-roasted almonds, boiled spinach
- Biotin (vitamin B7): egg yolk, beef liver, nuts and seeds
How many Frakenfoods or glutenoids do you think will contain even just one of these ingredients?

Gif source: https://tenor.com/bC9vy.gif
Keep in mind that whole food starches, fruits, and some vegetables also have the ability to increase blood sugars dramatically, so they’re not off the hook, either!
But they normally have more nutrients to provide and cause far less inflammation as long as blood sugars are stable.
Problem #2 – Taking More Insulin to Cover More Carbs May Create More Problems Than it Solves
Many diabetics are aware of how common it is for a consistent and higher load of carb intake to result in more chronic (long-term) hyperglycemic states.
Unfortunately, the majority of diabetics are not that good at calculating with 100% precision our diabetic medication doses while eating carb-rich meals.
In theory, this sounds great but let’s go over why this typically doesn’t work among a large majority of diabetics.
The more carbs per meal consumed the more insulin will be needed. This is the first step towards insulin resistance called hyperinsulinemia (13).
Insulin resistance occurs when the body does not respond as well to insulin as it once did, which typically leads to increased blood sugar levels.
After insulin resistance becomes present, it’s been observed that hyperinsulinemia may complicate blood sugar management further among type 1 and type 2 diabetics (14, 15).
One reason may be that insulin resistance can throw carb-counting off, making it more difficult to accurately dose medication for meals.
The more carbs consumed, the more insulin is needed, however the more accurate a diabetic will need to be with their medication dose for each of these meals.
Overall, there’s a greater likelihood of bigger medication doses leading to bigger errors that cause bigger blood sugar mistakes!
Below are examples of a couple of typical responses once insulin resistances begins with a type 1 diabetic.
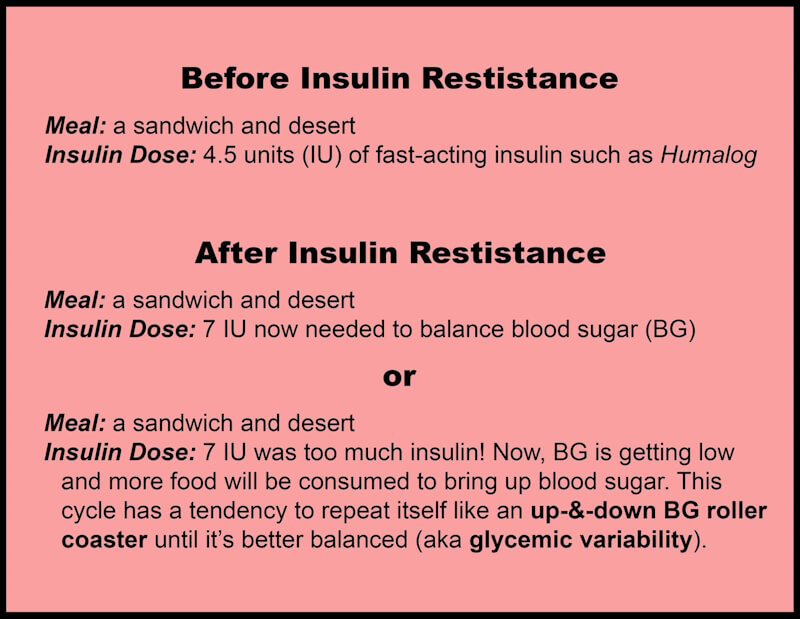
As expected, a diet heavy with ultraprocessed foods is associated with needing higher insulin levels most of the day (16).
Even if whole-food carbs were being eaten in larger portions, it would likely be a similar juggling act with calculating precise medication doses to balance those blood sugars, too.
What About Those Diabetics Who Can Eat Whatever They Want and Be “Fine” With Their Blood Sugars?
Although a small number of diabetics may be able to pull off a high-carb lifestyle along with a high dose of medication well enough, it’ll likely only be for a short period of time.
Research suggests their insulin resistance will likely increase due to hyperinsulinemia and the body’s sustained and impaired responses to it (17, 18).
Another important question I ask whenever this notion is brought up is, “What is ‘normal blood sugar’ to this diabetic?”
What’s “normal” blood sugar to some may be too high or low for others.
I will address these blood sugar standards in a later post.
Problem #3 – Chronic Blood Sugar Spikes & Roller-Coaster Blood Sugars (Glycemic Variability)
Blood Sugar Spikes
Blood sugar (BG) spikes are usually seen after particular foods are consumed, giving a sharp rise to BGs.
This and the blood-sugar-balancing roller coaster that typically follows should be avoided when possible among diabetics.
A big reason for the volatile blood sugars is due to a term that connects hyperinsulinemia to insulin resistance known as glucose toxicity.
Simply put, glucose toxicity is when impaired pancreatic beta cell (where insulin is produced) function occurs while experiencing high blood sugars.
This is caused by hyperinsulinemia and it can lead to reduced insulin secretion while increasing insulin resistance, resulting in long-term hyperglycemia risk (19).
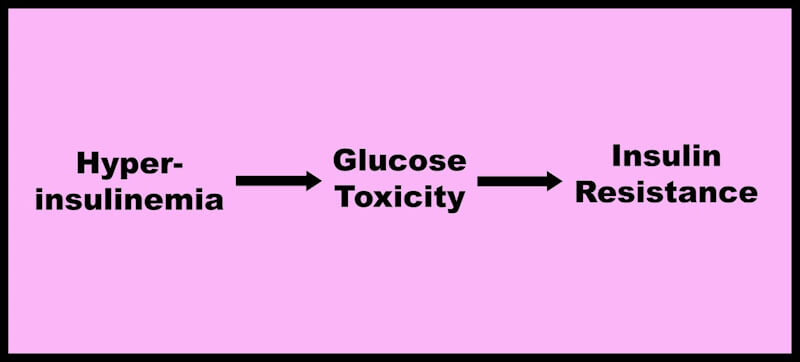
Not only that but it’s now generally accepted for glucose toxicity to be a major component in the worsening of diabetes and its management.
Glucose toxicity is suggested to create oxidative stress in the body, especially on the pancreas, leaving it and other organs dependent on the pancreas to become weaker and more susceptible to other complications.
Blood sugar spikes are known to commonly promote glucose toxicity (20, 21).
I’m sure many diabetics can relate to having experienced these blood sugar spikes after a carb-rich meal!
(Nachos, anyone?)
Blood Sugar Roller Coasters (Glycemic Variability)
Gif source: https://tenor.com/baFki.gif
The juggling act between high and low blood sugars, more commonly seen immediately after meals, is something all diabetics should also intend to avoid.
Glycemic variability is suggested to:
- be worse for endothelial function and oxidative stress when compared to solely, consistently high blood sugars (22)Endothelial function examples include blood clotting, helping immune response, regulating substances transferred from the blood to tissues
- expedite atherosclerosis development and cardiovascular disease (23)
- cause and worsen kidney dysfunction (24)
- increase the risk of diabetic retinopathy (25)
The list above accounts for the most common diabetic complications. Hopefully, it makes more sense why they’re widely seen among diabetics with chronically troubled blood sugars.
Lastly, let’s go over other inflammatory factors a carb-rich diet may influence.
Problem #4 – Other Inflammatory Variables
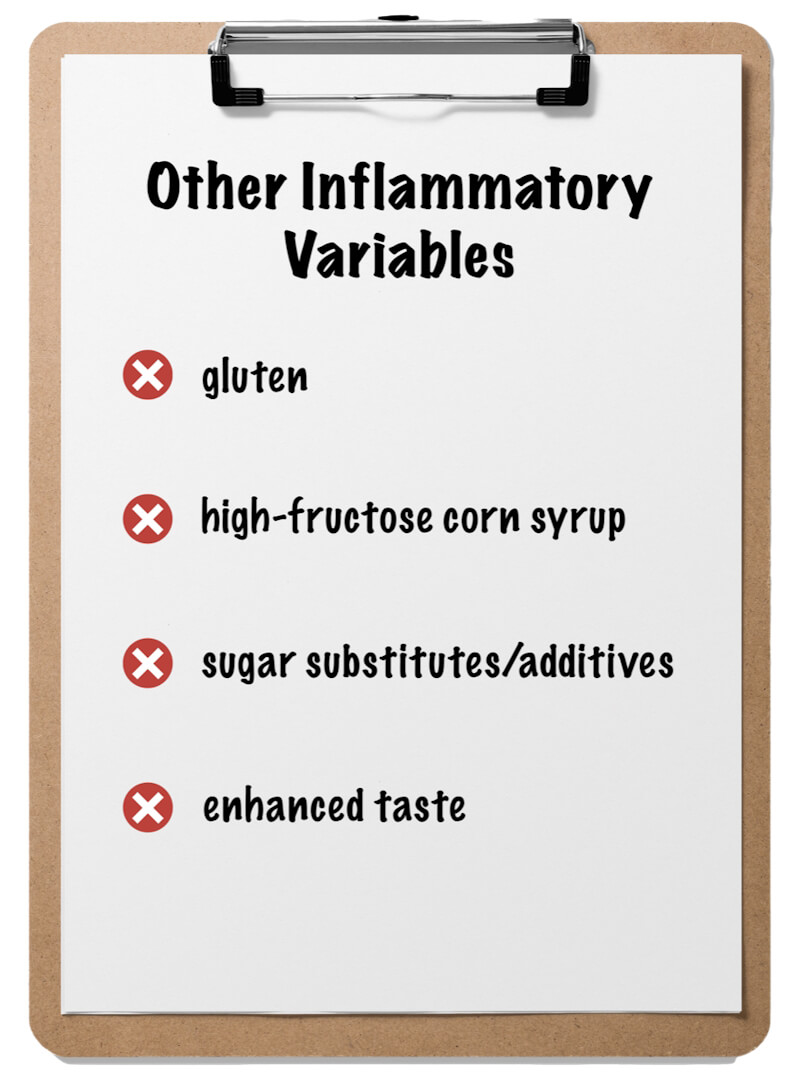
We’re now more aware of the direct blood sugar effects that a carb-rich diet may influence but unfortunately, the problems don’t stop here!
Let’s go over a short list of common Frankenfood traits and how they may impact diabetic health.
Gluten
I’ve written a definitive guide on specific factors of gluten that are associated with impaired autoimmune and diabetic health.
In summary, gluten is a protein found in many grains that is capable of altering immune function and nutrient absorption by attributing to a condition known as leaky gut.
Leaky gut is a gut disorder that compromises the gut lining, allowing pathological substances to pass through into the body, increasing illness risk and gut symptom risks.
In addition, leaky gut is more likely to occur among those with autoimmunity and may also be seen paired with chronic hyperglycemia (26, 27).
Although not every diabetic may be celiac or non-celiac gluten sensitive (NCGS), the risk for either of these conditions is considerably higher due to their already compromised immune system.
For the sake of blood sugar stabilization and likely inflammatory conditions present, I believe it would be safer than sorry to avoid gluten altogether.
High-Fructose Corn Syrup
High-fructose corn syrup (HFCS) is a widely used sugar-enhancer that makes food or drinks taste sweeter.
Examples include most sodas, conventional fruit juices, and many processed foods.
HFCS is often disguised by other names, such as:
- glucose–fructose
- isoglucose
- maize syrup
- glucose syrup
- fruit fructose
- crystalline fructose
- and more!
Upon consumption, HFCS skips normal digestive procedures and goes directly to the liver to begin fat production, which increases triglycerides and cholesterol but not before demanding a higher dose of insulin or diabetic medication to offset the likely blood sugar spikes.
Chronic HFCS intake has also been associated with leaky gut (28).
Sugar Substitutes

Sugar additives or substitutes aim to maintain a pleasurable taste while reducing caloric and/or sugar intake.
Some examples include:
- aspartame (NutraSweet, Equal)
- saccharin (Sweet’N Low)
- sucralose (Splenda)
- aspartame (diet sodas).
Sugar additives may also be associated with insulin resistance (29).
One theory behind this is that the “sweet” taste tricks the pancreas to release insulin when not actually needed. This frequency may impair insulin function.
It’s currently unclear how sugar substitutes may directly affect blood sugar management, however, research can validate its likely effect on overconsumption, which can then lead to blood sugar instability.
As with most things, especially diet related, the poison typically lies in the dose and the quality of these types of foods consumed.
Although there appears to be no direct blood sugar risk with the consumption of sugar substitutes, let’s see how these pleasurable tastes may increase overeating that typically lead to blood sugar problems.
How Favorable Tastes Influence Roller Coaster Blood Sugars
We mentioned that high-fructose corn syrup and sugar additives are used to make foods and drinks taste sweeter to consume.
This is a very common trait among processed junk foods.
These favorable tastes can lead to overconsuming a particular food or drink due to its ability to impair when you “feel full” (medical term: satiation), which confuses the body into thinking it’s still hungry when it shouldn’t be (30).
These foods just taste so good it makes it difficult to only eat a small portion and then easily stop.
Just think about it for a second.
Ever stop eating after just:
- 1 slice of pizza?
- 1 cookie?
- 1 M&M?
- 1 donut?
Of course, this typically leads to raised hyperinsulinemia and insulin resistance, which then influences hyperglycemic reactions (31, 32).

Gif source: https://tenor.com/bDKTr.gif
Why Convenient Foods Aren’t the Best Fit for Blood Sugar Stability
Life demands a lot.
Whether it’s school, work mandates, kids and their obligations, relationships, extended family, and sometimes all of these at once!
Oh, and don’t forget you also have to reign supreme with your diabetes management!
I get it. Believe me, I do. I’ve had type 1 diabetes since May 2000.
But can we step back for a second and spin some thoughts?
- Diabetics have impaired insulin function, right?
- Even among nondiabetics, blood sugar spikes and insulin resistance have been consistently noted with the consumption of highly processed junk foods that are normally high in carbohydrates, low in whole food ingredients, and low in nutrition.
- Given the fact that all diabetics are now entrusted to think and execute like their pancreas, why would we willingly want to make this job any harder than it already is by continuing to eat either a high amount of carbs, especially those that are ultraprocessed?
Don’t worry. I’m not pointing any fingers at anyone.
My dietary vice is some gluten-free pizza, maybe, 3 – 4 times a year! I blame my 2 younger sons for this.
I get there will be times when convenience foods will just be easier to acquire than having to go through all the prep work of providing yourself with more qualitative and blood-sugar-friendly options.
I will go over in an upcoming post how I address this for my own better blood sugar management.
Until then, please know there will always be a cause-and-effect relationship with every lifestyle choice you make as a diabetic.
I’m not saying this to darken the mood but I do believe it’s a reality that all of us diabetics need to accept.
And the sooner the better!
These choices will either enable or inhibit optimal diabetic health. Many of these harmful effects won’t be seen immediately, either.
And if they do spring up, it likely won’t be pretty given how many body cells are affected by chronic hyperglycemia.
The theme I want every diabetic to wrap their head around is that your pancreas is already dysfunctional! Stressing it and your calculated medication doses with a high-carb diet will likely avoid the consistent and reliable blood sugar results most diabetics seek.
Whether you agree or don’t agree with this notion is irrelevant because I want for you what you want for you.
The results are always showing us if what we’re doing is working.
After being a type 1 diabetic for 20+ years, I’m still figuring out new things that have helped my positive blood sugar results.
But I’ve also had many blundering failures!
Rome wasn’t built in a day and neither will you be.
And if you’re sick and tired of being sick and tired, not getting the blood sugar results you seek will not be acceptable!
In this next post, you’ll be learning how sleep loss may impair blood glucose levels.
Summary
- The amount of carbs isn’t the only factor that needs to be considered when it comes to successful blood sugar management. Others factors include:
- Carb quality: Are the carbs you eat highly processed and refined or whole foods? The more of a “Franken-food” it is, the more likely it will negatively impact BGs & your overall health, especially if it’s eaten routinely.
- Taking more insulin to cover more carbs: Remember, hyperinsulinemia leads to an increased risk of insulin resistance or worsening of it. When done in the long term, a significant number of body cells can become damaged due to the unstable effects this commonly has on blood sugars.
- Blood Sugar “Roller-Coasters”: too many blood sugar spikes, along with the ups and downs in attempting to stabilize once present, can further complicate insulin resistance and BG stability attempts.
- Other inflammatory variables: gluten, high-fructose corn syrup, sugar substitutes, and enhanced taste, can individually or collectively hinder blood sugar stability due to a varied amount of negative effects on optimal physiological function and increased likelihood of BG spikes.
References
2. Ultra-processed foods
3. https://jamanetwork.com/journals/jamapediatrics/fullarticle/2780512
4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8705763/
5. According to the studies included, 1.21-1.42 I2
6. Processed foods make us sick its time for government action
7. Study estimates two thirds covid 19 hospitalizations due four conditions
8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4119241/
9. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2757497
10. Ultra-Processed Food Consumption and Increased
11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8483964/
12. Blood glucose testing and control/hyperglycemia
13. https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-020-01688-6
14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7700208/
15. https://www.cdc.gov/diabetes/basics/insulin-resistance.html
16. As mentioned earlier due to, increased much of the day.
17. Insulin Resistance and HyperinsulinemiaIs
18. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6735759/
19. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2738809/
20. https://www.sciencedirect.com/science/article/abs/pii/S0026049523001154
21. https://pubmed.ncbi.nlm.nih.gov/30040822/
22. Oscillating Glucose Is More Deleterious to
23. https://www.ahajournals.org/doi/full/10.1161/CIRCRESAHA.120.316653
24. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8322551/
25. https://pubmed.ncbi.nlm.nih.gov/33252581/
26. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9271567/
27. https://www.science.org/doi/10.1126/science.aar3318
28. Avoid the hidden dangers of high fructose corn syrup video/
29. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7014832/
30. https://pubmed.ncbi.nlm.nih.gov/25988134/
31. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8705763/
32. Iatrogenic Hyperinsulinemia Not Hyperglycemia


