What if I told you that troubled and inconsistent blood sugars could be summed up in two words?
Insulin resistance.
We’ve all been told that insulin helps balance our blood sugars, but things can get messy when insulin resistance sets in!
How messy can it get, though?
Read on to find out how insulin resistance may impact:
- unstable blood sugars
- impaired bodily functions
- autoimmunity and
- type 1 diabetes
Ready?
Let’s rock n’ roll!
Too Long to Read Right Now?
Just give me your e-mail and I’ll send you the PDF version for you to read at your leisure (don’t worry, I won’t share your e-mail with anybody)!
Chapter 3
What Effects Can Insulin Resistance Have on Our Bodies?
Chapter 4
Why Only Increasing Your Insulin May Be More Damaging Than Helpful
Chapter 5
Is There A Link Between Insulin Resistance & Autoimmunity?
Chapter 6
Any Relationship Between Insulin Resistance & T1D?
Chapter 7
Dr. Mo’s Personal Experience with Insulin Resistance
What is Insulin Resistance?
Insulin resistance is a condition that doesn’t just affect people with diabetes.
It can be detected among those without diabetes, too (1).
Insulin resistance is when one doesn’t respond to insulin as effectively as they once did to balance their blood glucose levels properly.
Despite the right amount of insulin being produced or injected, glucose absorption or uptake is impaired, which usually results in higher blood sugars (aka hyperglycemia).
Chronic (long-term) hyperglycemia is commonly understood to be a significant precursor to type 2 diabetes.
However, many don’t realize that it may also further blood sugar troubles among type 1 and gestational diabetics.
A common comparison of insulin resistance is the key and lock example where:
- insulin = the key
- the body cells = the locks
During insulin resistance, the locks (body cells) become “rusty” or “change shape,” making it harder for the keys (insulin) to open them to transfer glucose to the cells from the blood.
As a result, blood glucose levels tend to increase, causing hyperglycemia.
I believe that insulin resistance is the backbone of most, if not all, of blood sugar management struggles.
If one can reduce all the factors influencing insulin resistance, they will likely have more consistent, reliable, and healthier blood glucose levels.
In the upcoming posts, I’ll explain how these different lifestyle choices are associated with insulin resistance and blood sugar instability.
Let’s first go over insulin resistance basics.
Why Does Insulin Resistance Occur?
Our bodies have many checks and balances to maintain internal balance.
The physiological term for this action is called homeostasis.
For example, when we are highly active for long periods, our body triggers thirst to signal us to drink some fluids to continue our current activity with more energy.
This helps to maintain balance during the body’s current needs.
One theory behind insulin resistance is that our bodies recognize that too much insulin can lead to low blood sugars (aka hypoglycemia), which triggers insulin resistance to disrupt the body’s ability to absorb insulin as intensely as instructed.
Simply put, insulin resistance is believed to be a protective response to consistently high insulin demands (2).
Conversely, others believe insulin resistance begins as the body becomes exhausted from these chronically high insulin demands (aka hyperinsulinemia).
Regardless of the correct theory, these consistent insulin spikes typically result from more-than-frequent carb-rich meals (3).
What makes matters worse is that consuming these hyperpalatable (delicious and commonly not as filling or nutritious) foods leads to even more insulin needed for the body cells to uptake this consumed glucose.
This then causes insulin resistance to worsen and a vicious circle to begin that is extremely common among type 1 diabetics.
(You’ll soon see why and how!)
Another cause for insulin resistance relates to energy balance.
You see, glucose is considered energy for the body.
Common energy-demanding examples include exercise, walking, running, yard work, cycling, etc.
However, if too much energy (glucose) is chronically consumed and unused, this may intensify insulin resistance, affecting many bodily functions.
Let’s make sense of this “energy balance” notion:
Imagine your body is like a thermostat in your home. Just as a thermostat keeps the temperature inside your house stable, your body works to stabilize the glucose levels in your bloodstream.
When you eat food, especially carbohydrates, your blood sugar levels rise, just like turning up the heat in your house.
Your body senses this increase in blood sugar. It takes action to bring it back to a stable level, just like the thermostat lowers the temperature to maintain a comfortable setting.
Depending on your current health status, insulin is released or injected and acts as the “thermostat” for your blood sugar, ensuring it doesn’t get too high.
This stability in glucose levels is crucial for providing a constant energy source to your cells, much like how a thermostat maintains a consistent temperature in your home.
The same goes for your body and performing some physical activity, regardless of intensity and duration.
If it doesn’t, your body typically becomes more insulin resistant when carb-rich meals are repetitive.
Routine physical activity is directly connected with making your body need less insulin to manage glucose (4).
What Effects Can Insulin Resistance Have on Our Bodies?
When insulin resistance runs wild with no intentions of stopping, bodily dysfunctions commonly occur!
The main reason is the strong connection between chronic insulin resistance and hyperglycemia.
And many of us already generally know that long-term hyperglycemia leads to many diabetic problems.
Something else to keep in mind is the following:
Let’s now go over a few of these diabetic issues from chronic insulin resistance.
Altered Hormones
The first problem we’ll review is a list of some hormones that commonly affect one another once this insulin-resistance line has been crossed.
Insulin is the primary hormone that is directly affected and for a quick review, remember that:
The longer you have high insulin demands, the more resistant your body will likely become to it (unless you’re a high-powered athlete but I’ll discuss this in another post soon!).
So, let’s continue with a few other hormones typically affected by insulin resistance that make blood sugar management more difficult.
Glucagon
Insulin resistance can disrupt the balance between insulin and glucagon, another vital hormone in glucose metabolism.
Glucagon’s function is to raise blood sugar by releasing stored glucose from the liver.
In a healthy, non-diabetic, glucagon acts in response to blood sugars dropping due to:
- fasting for an extended period
- exercise gobbling up all the glucose/energy in your blood and muscles
Because type 1 diabetics (T1Ds) have trouble getting glucose into their bodies, this is interpreted as if we have low blood sugar and need glucose to raise it.
Similar to a long fasting session.
Sometimes, glucagon can become more dominant than insulin, fueling high blood sugars.
Leptin
Leptin is a hormone produced by fat cells that helps to regulate energy balance by signaling to your body that you’re “full” from your meal(s).
Its primary function is to prevent overeating.
Insulin resistance is often associated with leptin resistance, where the body doesn’t respond appropriately to leptin’s signals (5).
This can lead to increased appetite and weight gain.
Whenever I think about leptin resistance, I think about when I worked in an Italian restaurant in Orlando.
There was free bread we would give our guests, and of course, most of them also ate pasta. Many also had wine with their meals.
Many of these guests were obese, as well!
Just from the bread, pasta, and wine alone, this is enough not only to shoot up insulin demands but, if these meals are routine, can also impair leptin function, leading to these guests consuming much more food than their bodies should comfortably be eating.
This then cues a vicious circle between insulin and leptin resistance!
Cortisol
Cortisol is the primary hormone most commonly associated with stress.
When a stressful event occurs, our body interprets this as a “fight” or “flight” scenario, i.e. we’re either going to fight this danger or threat or run away from it.
To accomplish this effectively, our bodies release cortisol, which then activates glucose release into the blood so that we have enough energy to fight or flee.
Nowadays, mental and emotional stressors appear to be more common than physically threatening ones (6).
However, your body will respond no differently!
Chronic insulin resistance is often associated with an overactive stress response, leading to elevated cortisol levels and glucose release (7).
High cortisol levels may also worsen insulin resistance (8).
Do you hear “vicious circle” echoing in the background?
Sex Hormones

Just like insulin and glucagon can become imbalanced during insulin resistance, the same can occur with sex hormones, particularly estrogen and testosterone.
Estrogen and testosterone are both produced in the ovaries in females and testes in men.
However, females typically produce lesser amounts of testosterone. Similarly, men generate minor estrogen levels.
Estrogen
Estrogen’s primary functions are to (9):
- regulate the growth, development, and physiology of our reproductive system
- influence the neuroendocrine, skeletal, fat, and cardiovascular systems
High insulin levels may stimulate the ovaries to produce more testosterone, which can be converted into estrogen in the body tissues (10).
These insulin and estrogen imbalances can lead to conditions such as polycystic ovary syndrome (PCOS), characterized by irregular menstrual cycles, infertility, and symptoms of high androgen levels like acne and hair growth (11).
Additionally, insulin resistance typically contributes to weight gain, which increases estrogen production in fat tissue. This may worsen this sexual hormone imbalance and its symptoms.
This hormonal dysregulation may also increase the risk of estrogen-sensitive conditions like certain types of breast and endometrial cancers (12).
Testosterone
Some testosterone functions include the ability to:
- increase bone density
- establish proper muscle size and strength
- stimulate sexual desire (aka libido)
- assist with optimal fat distribution
- help drive puberty in males
- produce red blood cells
As previously mentioned, testosterone can be converted into estrogen, which can lead to hormone imbalances, weight gain, and reduced function with everything just listed above.
But how does this occur?
- Insulin regulates the hypothalamic-pituitary-gonadal (HPG) axis, which controls testosterone production (13).Because insulin function is impaired during insulin resistance, one of the effects may be reduced testosterone production.To minimize confusion and clarify what I previously stated, insulin resistance may increase testosterone production in the ovaries while decreasing production in the testes.
- It’s extremely common for body fat to increase as insulin resistance worsens, specifically visceral (relating to the organs in the chest and abdomen) fat.Fat tissue contains an enzyme called aromatase that converts testosterone into estrogen.Aromatization also spikes up as body or visceral fat increases (14)!As a result, insulin and leptin resistance are also directly influenced.Do you see a vicious circle light up in your head again?
Insulin resistance may also cause erectile dysfunction.
Three factors that make erections possible are (15):
- testosterone
- adequate blood flow through the corpus cavernosum
- proper nerve function
As we’ve already gone over, insulin resistance may damage blood vessels and nerve function while impairing adequate testosterone levels (16).
Adiponectin
Adiponectin is a hormone released by fat cells and helps regulate blood glucose levels, fat metabolism, and insulin sensitivity (17).
Insulin resistance is often associated with lower adiponectin levels, encouraging even more insulin resistance (18).
You already know what I’m going to say, don’t you?
Gif source: https://tenor.com/HAu4.gif
Low Energy
As you would feel after a long race, our bodies can feel tired when we can’t get enough sugar inside our cells.
Even though we may be eating enough food, our cells aren’t getting the energy they need because insulin resistance prevents glucose from entering them correctly.
As a result, one of the potential symptoms that may follow is the feeling of tiredness and sometimes even dizziness (19).
I share a very similar story that many other type 1 diabetics have with these shallow levels of energy just before learning I had type 1 diabetes!
Continued Hunger

Insulin plays a smaller role than leptin in managing hunger by signaling the brain when enough energy is available and reducing the desire to eat (20).
However, among insulin-resistant individuals, this feedback loop is disrupted (21).
Despite elevated insulin levels needed to transfer glucose from the blood properly, the signal is not received, leading to perceived energy deficiency.
As a result, the brain doesn’t get the message that enough food has been eaten. This disconnect continues to fuel hunger signals, often leading to overeating.
We know insulin helps transport glucose from the bloodstream into the cells for energy. Still, less glucose is transferred when insulin resistance is present, causing higher blood sugar levels and triggering increased hunger.
If carbs have been the primary macronutrient of consumption (the others being protein and fat), the body usually craves more food, particularly carbohydrates, to produce more energy.
Overconsumption of these high-calorie/low-nutrient foods will also further enable insulin resistance due to the higher insulin demands and potential frequency of these foods being consumed.
Of course, insulin and leptin signaling are now both thrown off, leading to….
…you guessed it! Another vicious circle.
Weight Gain
If glucose or energy can’t be stored in our body cells, our digestive system will transfer any excess glucose to our fat cells (22).
This is why most exclusive type 1 diabetics generally are not capable of gaining weight right away after their diagnosis.
It’s not to say we can’t but it may take some time.
However, there is medical research suggesting that (23):
- 62% of adult T1Ds are overweight or obese compared to
- 64% of obese or overweight adults without diabetes and
- 86% of overweight or obese type 2 diabetics
Weight gain, especially rapid weight gain, can also lead to an increased demand for insulin production.
Our fat and muscle cells will naturally accommodate these elevated insulin signals.
The catch, however, is that they can’t keep up with it forever!
- There’s only so much gas you can fill in your car
- Only so much fluid you can fill your cup to drink from
- Only so much food you can consume and ingest
Hyperinsulinemia can stress the insulin-producing beta cells in the pancreas, leading to their eventual exhaustion and reduced insulin secretion.
Moreover, overeating, particularly high-sugar foods, can cause blood sugar spikes.
Over time, these repeated spikes can desensitize the body’s cells to insulin, further promoting insulin resistance.
Do you see how this impaired insulin production and altered glucose uptake by the body cells can lead to (say it with me now) another vicious circle?
These two mechanisms feed into one another!
Cardiovascular Dysfunction & Disease
High Blood Pressure
Under normal conditions, insulin helps regulate the balance between the opening and closing of blood vessels when the heart pumps blood.
However, this balance becomes impaired when insulin resistance is present, typically leading to higher blood pressure (24).
But how?
Some ways insulin resistance may impair blood pressure are as follows:
- Insulin resistance disrupts the body’s ability to relax blood vessels and regulate sodium, leading to higher blood pressure.
- It can increase the sympathetic nervous system (aka fight or flight) activity, causing blood vessels to constrict more.
- Insulin resistance is associated with inflammation and oxidative stress, which can damage blood vessels and influence higher blood pressure.
- Over time, the pancreas may overproduce insulin to compensate for resistance, raising blood pressure.
- Lastly, insulin resistance can lead to endothelial dysfunction, disrupting blood pressure regulation.
The exact blood pressure mechanisms of influence remain an active research topic.
Dyslipidemia (High Cholesterol &/or Fats)
Insulin resistance has also been linked to dyslipidemia in the form of (25):
- increased low-density lipoproteins (LDL; bad cholesterol)
- elevated triglycerides
- low levels of high-density lipoproteins (HDL; good cholesterol)
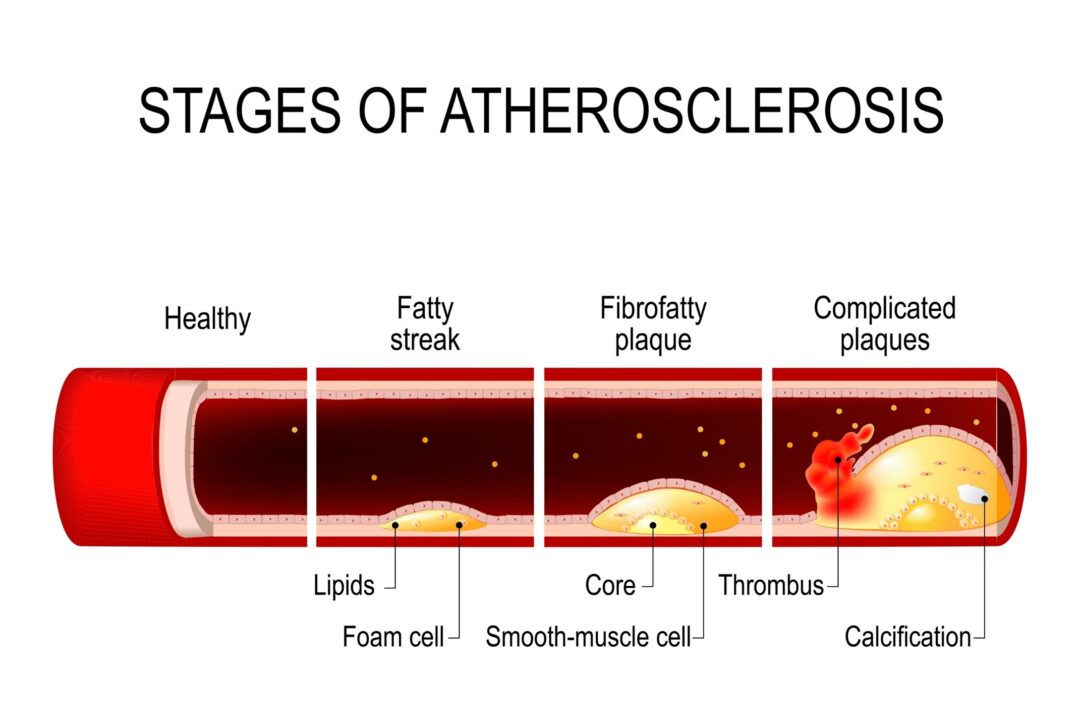
When dyslipidemia continues and worsens, it can build up plaques in the arteries (aka atherosclerosis).
These plaques can narrow the space where blood flows through in the arteries.
If this narrowing worsens, it may reduce blood flow, and these plaques may also break open and lead to blood clots.
This typically influences higher blood pressure, as well.
Heart Failure
By nature, insulin resistance is an inflammatory response.
As a result, it may contribute to the arteries bulging (aka aneurysm) rupturing, causing a heart attack (26).
Another way this may occur is due to insulin signaling being altered among the cardiomyocytes.
These cardiomyocytes are responsible for the heart contractions that help pump blood throughout the body.
Insulin resistance can alter these cardiomyocytes’ performance, which may become another factor leading to higher blood pressure and/or a heart attack (27).
Kidney (Renal) Dysfunction
Insulin resistance may significantly impact kidney function, leading to potential renal damage over time.
Insulin resistance can cause high glucose levels to remain in the blood, damaging millions of tiny filtering units inside your kidney (aka nephrons).
As a result, these nephrons may respond by growing thick and becoming scarred over time (28).
Eventually, the kidneys may leak essential proteins into the urine instead of keeping them in the blood, a condition known as proteinuria (29).
This is an early sign of kidney disease.
If high blood pressure is also present, it can damage the blood vessels in the kidneys, making them less effective at filtering out waste from your blood.
(Hopefully, a vicious circle is popping up in your head right now!)
Though insulin resistance is a protective response, it’s still an inflammatory trigger with many negative consequences, especially if nothing is being done to calm it down!
I’ve already mentioned that insulin resistance normally activates oxidative stress, an inflammatory response.
The longer this inflammation remains intact, the more damage it can cause.
So, add “causing harm to the kidneys” to the list of other things oxidative stress may also impair (30).
Compromised Nerve Function
Earlier, I stated that proper nerve function is needed for healthy erections.
Insulin resistance may also impair the nerves in our bodies by altering their metabolism and function, contributing to nerve damage or neuropathy (31).
Nerve damage may occur via various mechanisms, which may overlap with insulin resistance symptoms, such as (32):
- increasing oxidative stress
- promoting inflammation
- causing the formation of advanced glycation end products (aka AGEs), which means sugar gets stuck on protein or fat cells in the body that then usually causes dysfunction among them
Nerves thrive when they are preserved and well-maintained.
A diet and lifestyle filled with antioxidants, nutrient-dense foods, physical activity, and quality sleep are a few factors that help to nourish our nervous system.
Also, note that because insulin resistance often accompanies dyslipidemia, an abnormal amount of cholesterol and/or fat in the blood may increase free radical production.
These free radicals are the foundation of why oxidative stress exists, which can harm the nerve cells, among a host of others.
Furthermore, insulin has neurotrophic effects, meaning it promotes nerve growth and health.
Insulin resistance reduces these beneficial effects, which may lead to more nerve damage.
Yup. Vicious circling is nonstop with insulin resistance!
Eye Trouble (Retinopathy)
Chronic insulin resistance, hyperinsulinemia, and hyperglycemia may trigger a cascade of detrimental effects on the retina.
Prolonged insulin resistance can damage the retina’s tiny blood vessels or capillaries, causing them to leak or become blocked, thereby reducing the blood supply to retinal tissues (33).
We know chronic hyperglycemia can promote inflammation and oxidative stress, but these two processes can also damage the retinal tissue and contribute to the progression of retinopathy (34).
This chronic inflammation may also activate several damaging pathways, leading to abnormal retina blood vessels, a severe form of retinopathy known as proliferative diabetic retinopathy.
Insulin resistance’s frequent association with dyslipidemia may worsen hyperglycemia’s effects on the retinal blood vessels, accelerating the development of retinopathy (35).
Faster Aging with Quicker Wrinkles!
First, chronic hyperglycemia may cause collagen and elastin glycation, the skin’s main structural proteins.
These AGEs cause cross-linking of collagen and elastin fibers, making the skin lose its elasticity and forming wrinkles (36).
Second, because chronic hyperglycemia increases oxidative stress and free radical production, these free radicals may damage skin cells, worsen inflammation, and degrade collagen, all of which accelerate skin aging (37).
Third, in addition to free radicals and oxidative stress, insulin resistance is also associated with increased levels of inflammatory cytokines (38).
Cytokines are small, pro-inflammatory proteins vital in the growth and activity of immune and blood cells.
In other words, when active, they signal the immune system to get to work!
There’s a strong association between elevated cytokines and aging where their overproduction increases the risk of (39):
- reduced collagen and skin thickness
- increased capacity to bruise with a longer recovery time
- overall reduced skin immunity function
Chronic inflammation, yet again, can damage the skin structure and impair the skin’s ability to repair and regenerate itself, accelerating the aging process (40).
Why Only Increasing Your Insulin May Be More Damaging Than Helpful

It’s extremely rare to find a type 1 diabetic who has experienced a smooth transition between their lifestyle and healthy, sustainable blood glucose levels within weeks of their diagnosis.
Especially for those diagnosed at a younger age and beyond.
The typical response is to continue living as one did before their T1D diagnosis, yet it’s likely that some or all of these lifestyle factors may have encouraged their autoimmunity.
As a result, based on personal experience, I believe that lifestyle factors need to be polished up for better blood sugar management results.
At the time of this writing, conventional medicine isn’t able to address these lifestyle triggers properly under the present health insurance model.
This is only because more time and energy need to be spent educating and helping those out of their unhelpful routine that, for some, is the only way they have known their whole life!
As a result, our doctor’s typical response to chronically high blood sugars is to increase diabetic medication doses, be it insulin or pills.
But is this actually helping?
There are many studies suggesting how increased insulin demands are associated with (41, 42, 43):
- more insulin resistance
- weight gain
- hypertension (high blood pressure)
- hypercholesterolemia (high cholesterol)
- higher triglycerides
This list of reactions is collectively known as metabolic syndrome and these symptoms are widespread among diabetics (44, 45).
Keep in mind, the noted research above was among nonobese, nondiabetics!
So, if this is all capable of occurring in nondiabetics, it should make more sense that many diabetic complications are commonly found with higher insulin demands, as well.
These include but are not limited to (46, 47, 48, 49, 50, 51):
- obesity
- cardiovascular disease
- polycystic ovary syndrome (PCOS)
- diabetic nephropathy (kidney disease)
- diabetic neuropathy (nerve disease)
- depression
- diabetic retinopathy (impaired vision)
Incidentally, it should come as no surprise that hyperinsulinemia is also likely to lead to more frequent states of hyperglycemia and inflammation (52).
How bad can this inflammation get, though?
Is There A Link Between Insulin Resistance and Autoimmunity?

We just learned how insulin resistance may cause dysfunctions in a diabetic body.
To make matters worse, did you know the one thing that all diseases, illnesses, and sicknesses have in common is chronic inflammation?
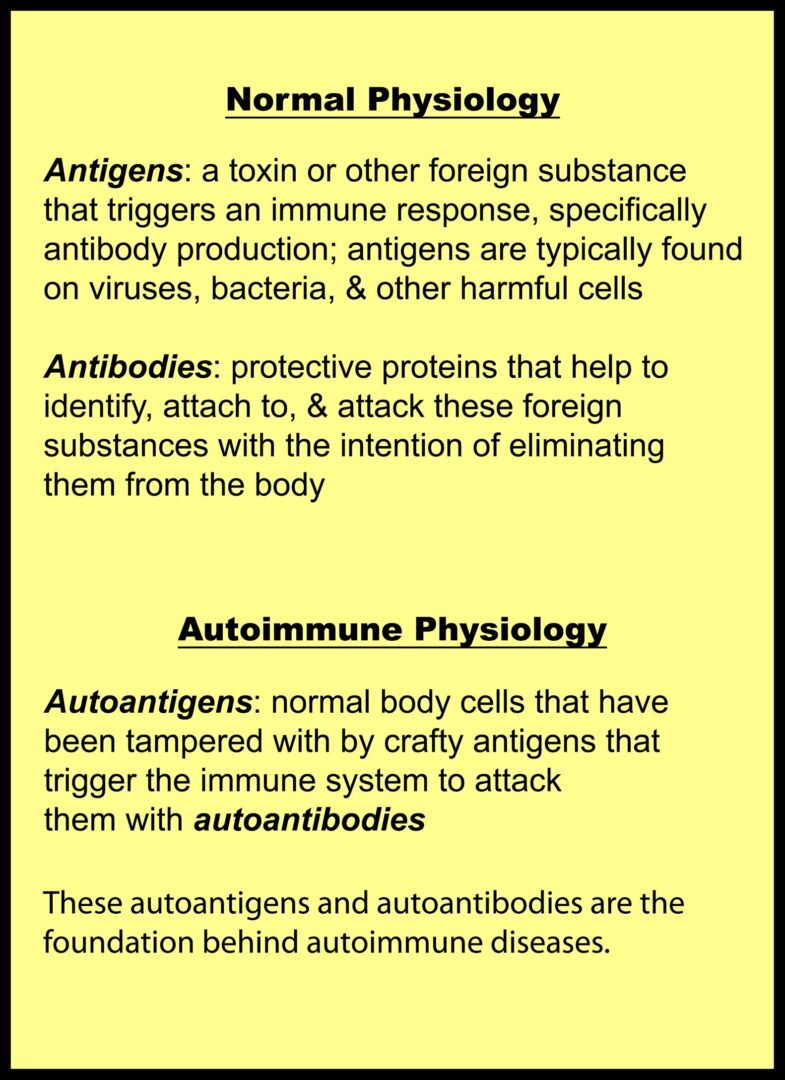
Autoimmunity is a complex process where the immune system mistakenly targets the body’s tissues, leading to various autoimmune diseases like rheumatoid arthritis, multiple sclerosis, and/or type 1 diabetes.
Insulin resistance triggers a chronic inflammatory state due to the excessive production of pro-inflammatory cytokines and oxidation.
Remember that cytokines are pro-inflammatory proteins that trigger the immune system to battle present inflammatory variables poking around.
These cytokines, such as TNF-α, IL-6, and IL-1β, are known to be involved in the development and progression of several autoimmune diseases.
For instance, TNF-α and IL-6 promote differentiation and function among diabetic immune cells and are believed to favor type 1 diabetic onset and progression (53).
Additionally, insulin resistance also affects the immune response by impacting immune cell functions (54).
During insulin resistance, there is an increased activation of the innate immune system and a corresponding reduction of the adaptive immune response.
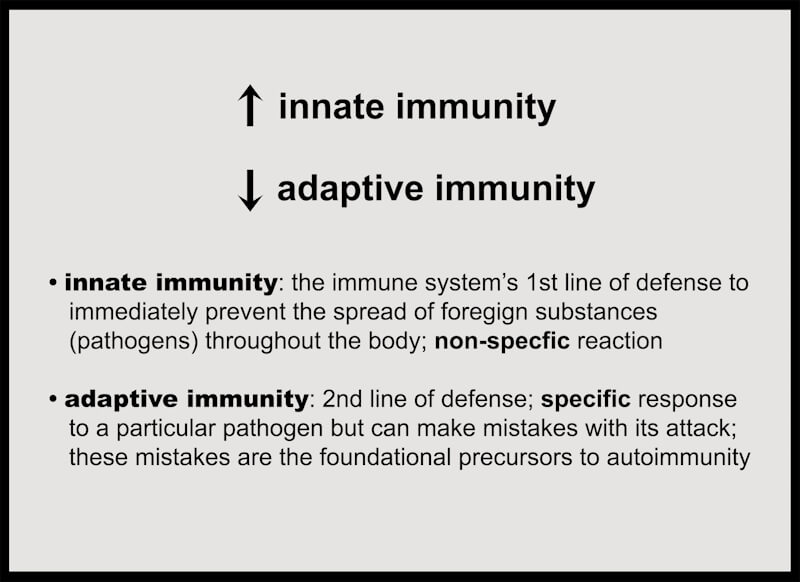
This immune dysregulation leads to persistent immune activation and hyper-responsiveness, which may contribute to the breakdown of immune tolerance to autoimmune triggers, a critical step in the development of autoimmunity.
Furthermore, the chronic inflammatory stress from insulin resistance could increase the expression of heat shock proteins (HSPs).
Quote taken from: https://link.springer.com/article/10.1007/s12192-022-01314-9
HSPs, while protective under normal conditions, can become targets of the immune system in a pro-inflammatory state, producing autoantibodies against them, another factor that may trigger autoimmunity.
(I’ll review autoantibodies in just a second, so hang tight!)
Any Relationship Between Insulin Resistance and Type 1 Diabetes?
As many of you already know, type 1 diabetes (T1D) is an autoimmune condition characterized by the destruction of insulin-producing beta cells in the pancreas, leading to impaired insulin production.
This requires using prescribed insulin to regulate our blood glucose levels better.
Autoimmunity in T1D is driven by the immune system’s mistaken recognition and attack of these pancreatic beta cells.
The connection between insulin resistance and T1D is a complex and active area of research.
Although there is no current, direct connection between insulin resistance and type 1 diabetes, I’m sure you all will be able to appreciate insulin resistance’s effect on various bodily functions that likely won’t help stop T1D from developing!
In most cases, insulin resistance is linked to obesity and type 2 diabetes (T2D) development, where cells fail to respond appropriately to insulin.
However, a phenomenon known as “double diabetes” is increasingly recognized, where individuals with type 1 diabetes also exhibit insulin resistance (55).
As previously mentioned, I believe that the everlasting state of insulin resistance is the main culprit behind chronic hyperglycemia and blood sugar mismanagement among the type 1 diabetic population.
Furthermore, insulin resistance may contribute to a more rapid loss of beta cells in T1D through glucotoxicity, where high blood glucose levels, combined with insulin resistance, intensify beta cell stress and apoptosis (56, 57).
Don’t forget that insulin resistance also increases insulin demand, which is another way beta cell stress and dysfunction may become more problematic.
There is also a theory that assumes among individuals genetically predisposed to type 1 diabetes, insulin resistance might increase the expression of specific autoantigens, making them more likely targets for autoimmunity, thereby enabling the onset of T1D.
Emerging research suggests that insulin resistance may indirectly influence the course of autoimmunity and type 1 diabetes.
Therefore, interventions to reduce insulin resistance might modify the progression of T1D.
Dr. Mo’s Personal Experience with Insulin Resistance
Given how much I’ve experimented with my body’s ability to respond to insulin, it is my experience to know that insulin resistance can change rather quickly, for better and for worse.
Five main factors may play into insulin resistance, as you’ll soon read in the following posts:
- Diet
- Sleep
- Activity
- Stress
- Gut health
My blood sugars won’t be a problem if my positive lifestyle choices remain consistent.

Image source: Dr. Mo’s colleague performing dry needling on his recovering knee (& yes, Sesame Street kicks major butt!)
However, after a couple of recent surgeries (at the time of this writing), having two kids, and other miscellaneous family, work, and life challenges and demands, I’ve noticed insulin resistance creep back in expectantly.
Truthfully, my type-A personality fits well with my diabetes because my repetitive habits help to keep positive diabetic outcomes consistent and reliable.
But while recovering from these surgeries over the past year, I have noticed my blood sugars spike back up a bit while not responding as well to my usual course of insulin injections (aka boluses).
The main reason I believe this is occurring is that I’m currently struggling to keep up with my gut health protocols, in addition to my activity levels having severely dropped out of routine while I rehab my knee and shoulder.
I’m slowly getting my groove back but consistency is vital to maintain the benefits of stable blood sugars.
As many of you now know, insulin resistance, hyperinsulinemia, and hyperglycemia are commonly interchangeable and feed into one another more so if there has been no intention behind altering either one or all.
In other words, it’s not likely to have one without the other!
This is something I wish someone told me 20+ years ago when I was diagnosed with type 1 diabetes.
Although I was 18 years old and felt like I was still invincible, I may not have considered the severity of this statement or had any intention to improve it as seriously as I do now.
This is why our environment plays a heavy role in how a type 1 diabetic will manage their blood sugars, especially among kids who have it!
So, lead well and with intention, parents!
But this is a topic for another post!
Summary
- Insulin resistance doesn’t just affect type 2 diabetics. It can also affect nondiabetics and when type 1 diabetics are conflicted with it, it’s called double diabetes.
- Insulin resistance occurs when the demand for insulin continues to be higher than the body recognizes to be reasonable (aka hyperinsulinemia), making it more difficult for the body to utilize insulin optimally.
- The long-term effects of insulin resistance are plagued with diabetic complications, along with metabolic disorders and weight gain, while directly aiding in chronic inflammation in the body.
- Simply giving yourself more insulin will likely just make insulin resistance worse since this is the reason for it existing in the first place.
- Insulin resistance increases innate immunity (the first line of defense) while reducing adaptive immunity (the second line of defense that is prone to mistakes when not functioning correctly; a common trait of chronic inflammation.
References
1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5912218/
2. https://diabetesjournals.org/diabetes/article/64/3/673/40358/Insulin-Resistance-as-a-Physiological-Defense
3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4338588/
4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5569266/
5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6354688/
6. https://www.mentalhealth.org.uk/explore-mental-health/statistics/stress-statistics
7. https://link.springer.com/article/10.1007/s12011-018-1629-y
8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5115704/
9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3389841/
10. https://journalofmetabolichealth.org/index.php/jmh/article/view/50/184
11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8564180/
12. https://pubmed.ncbi.nlm.nih.gov/35145826/
13. https://pubmed.ncbi.nlm.nih.gov/7852532/
14. https://pubmed.ncbi.nlm.nih.gov/11399122/
15. https://www.ncbi.nlm.nih.gov/books/NBK513278/
16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3877124/
17. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8066826/
18. https://pubmed.ncbi.nlm.nih.gov/23266767/
19. https://www.diabetes.co.uk/tiredness-and-diabetes.html
20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1642707/
21. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4587882/
22. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6832997/
23. https://publichealth.jhu.edu/2023/overweight-and-obesity-in-people-with-type-1-diabetes-nearly-same-as-general-population
24. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3996172/
25. https://cardiab.biomedcentral.com/articles/10.1186/s12933-018-0762-4
26. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8850393/
27. https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.116.306206
28. https://www.mountsinai.org/health-library/diseases-conditions/diabetes-and-kidney-disease
29. https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-021-02934-y
30. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7007944/
31. https://www.cdc.gov/diabetes/library/features/diabetes-nerve-damage.html
32. https://pubmed.ncbi.nlm.nih.gov/18473845/
33. https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy
34. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1880867/
35. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4063092/
36. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4082166/
37. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5643203/
38. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2246086/
39. https://pubmed.ncbi.nlm.nih.gov/23659624/
40. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4082166/
41. https://academic.oup.com/jes/article/3/9/1727/5537533
42. https://www.sciencedirect.com/science/article/abs/pii/S093947530700110X
43. https://www.metabolismjournal.com/article/S0026-0495(12)00359-9/
44. https://diabetesjournals.org/care/article/28/8/2019/23775/Metabolic-Syndrome-in-Type-1-DiabetesAssociation
45. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7721212/
46. https://www.mdpi.com/1422-0067/22/15/7797
47. https://www.thieme-connect.com/products/ejournals/abstract/10.1055/s-2007-1016294
48. https://www.karger.com/Article/Abstract/93632
49. https://academic.oup.com/endo/article/152/10/3638/2457143
50. https://journals.sagepub.com/doi/pdf/10.1177/11795514221090244
51. https://pubmed.ncbi.nlm.nih.gov/28575111/
52. https://my.clevelandclinic.org/health/diseases/24178-hyperinsulinemia
53. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7074462/
54. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6925764/
55. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3671104/
56. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3608918/
57. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2738809/


