One of the first recommendations many physicians give to their newly diagnosed or struggling type 1 diabetic patients is to improve their diet.
But how will this recommendation improve your blood glucose levels?
Read on to learn:
- Why stressing out a dysfunctional pancreas isn’t such a good idea (despite this being a common request)
- Low-carb pros & cons
- Finding answers to the low-carb cons
- Why food quality matters with insulin sensitivity and better blood sugars
Let’s get to it!
Why a Low-Carb Diet is a Great Start for Stable Blood Sugars
Reduced Carb Intake

In my High Blood Sugar Causes series, I detail what causes insulin resistance and why this can be problematic for stable blood glucose levels, especially if one is looking for consistency.
One of the main takeaways is that the more insulin demand increases, the more resistant our cells will likely become to insulin (1).
This makes blood sugar management more complex and less predictable.
There are only three macronutrients that can be consumed:
- Proteins
- Fats
- Carbohydrates
Carbohydrates can increase blood sugars (BGs) depending on the amount and quality, whereas protein can also increase BGs at a slower and more predictable rate.
Fats, alone, don’t typically have much effect on carb metabolism. Still, mixed with high-carb foods, e.g., nachos, pizzas, pasta, etc., this commonly delays glucose absorption and causes unstable blood sugars.
With carbs being the primary driver behind blood sugar increases, reducing this macronutrient will likely be a positive step in the right direction.
Here’s why.
Dr. Bernstein’s Law of Small Numbers
Image source: https://www.diabetes-book.com/about/https://www.facebook.com/photo/?fbid=199178128271247&set=a.199178114937915
Here’s a common scenario many diabetics have experienced:
- Pancreas malfunctions, leading to impaired insulin function and diabetes.
- Many of us are told to make sure there’s enough diabetic medication (insulin or pills) to cover what we’re eating, and everything will be just fine.
- We’re far from “just fine” or know our blood sugars could be managed better, but we’re stuck!
Dr. Richard Bernstein is an MD who’s had type 1 diabetes since he was 12 years old (1946) and is currently without any diabetic complications or ill health at his current age.
He follows a strict diet regimen that you can read about in his Diabetes Solution book (2).
This accomplishment is no small task, given how demanding diabetic management can be!
The foundation of Dr. Bernstein’s blood glucose management lies in his Law of Small Numbers.
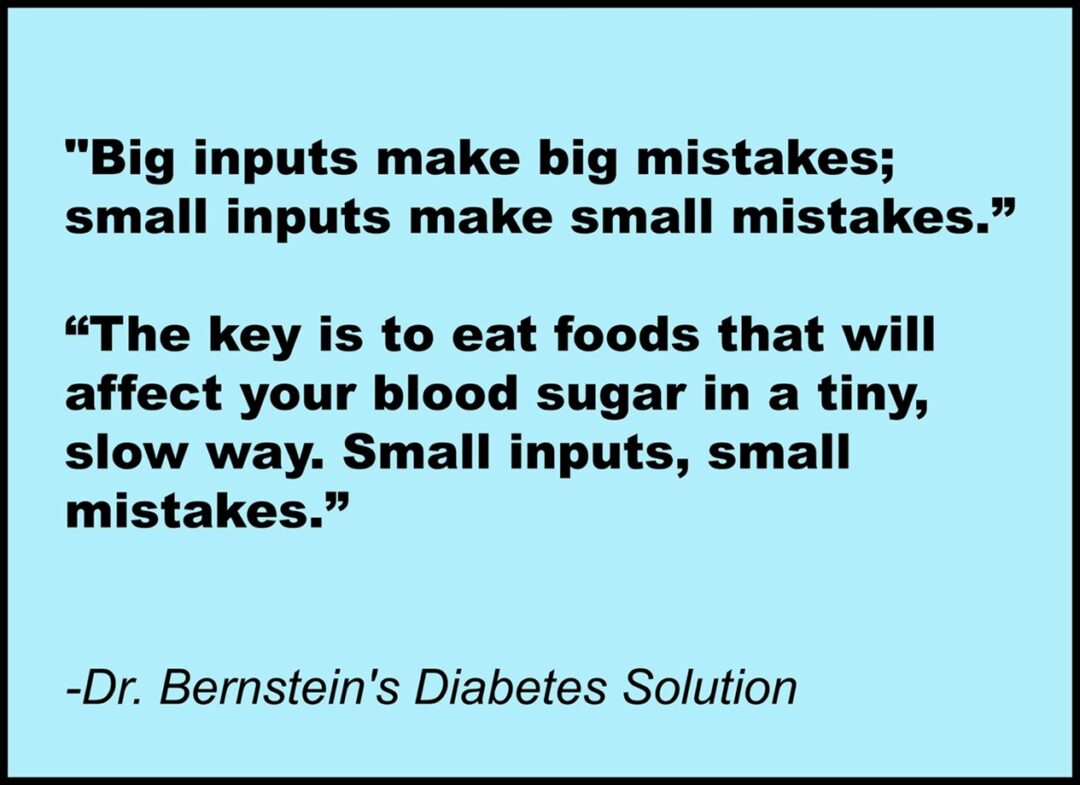
In other words, the less insulin you demand, the fewer headaches you’ll likely juggle to manage your BGs better.
The simplest way to minimize insulin demand is to eat a low-carb/high-protein diet.
This concept is so unbelievably simple that it’s silly that this isn’t the foundation of what we’re taught when first learning how to manage our blood glucose levels.
Increased Protein Intake
Many individuals are not aware of the fact that protein does increase blood sugars, as well!
However, it does so at a much slower and predictable rate (3, 4).
Making this your primary macronutrient of consumption will encourage you to reduce your insulin demands for your meals.
Another benefit of eating more protein is that you feel full quickly and for longer periods of time.
This is a fantastic tool to have especially for those who snack frequently with resulting blood glucose chaos.
Lower Insulin Demands
Now that carb intake has been reduced, the demand for insulin will likely do the same.
There are two benefits to this.
More Insulin Sensitivity
With limited carb intake, insulin’s need to overextend itself is also reduced.
The medical literature shows that increased insulin demands increase insulin resistance risk (5).
So, it makes sense that the opposite will occur when insulin demand drops (6).
Diabetic Management Cost Savings
Listen up if you’re burning through insulin vials every 1 – 2.5 weeks!
The more you reduce your insulin demands for carb-heavy meals, the more insulin sensitive you’ll likely become.
This will leave you needing less insulin in your fridge, diabetic gear, and body!
 Gif source: https://tenor.com/bH1a0.gif
Gif source: https://tenor.com/bH1a0.gif
You’ll not need to go through as many infusion sets and reservoirs if you’re an insulin pump user, either.
If you do insulin injections, your demand for syringes will also drop.
Hopefully, you can see where this positive snowball is rolling!
Let’s top off this good news with Eli Lilly, which produces Humalog insulin, dropping its cash price to $35/vial in 2023 (7).
This is a massive step in the right direction for those who need insurance or have less-than-desirable health plans.
Successfully attaining insulin sensitivity will likely save you on your diabetic management costs.
This can help manage your diabetic management stress, as well!
Decreased Rollercoaster Blood Sugars (aka Glycemic Variability), Overeating, & Weight Loss
Glycemic variability is based on how often your blood glucose level changes throughout the day.
The goal is to keep this as stable and calm as possible.
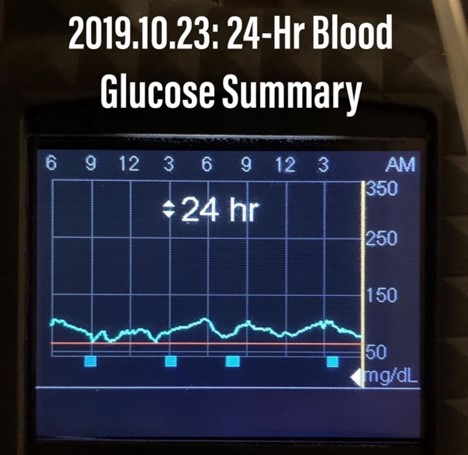 Image source: Dr. Mo’s Instagram page
Image source: Dr. Mo’s Instagram page
Think of having as close of a flatline of blood glucose levels in 24 hours.
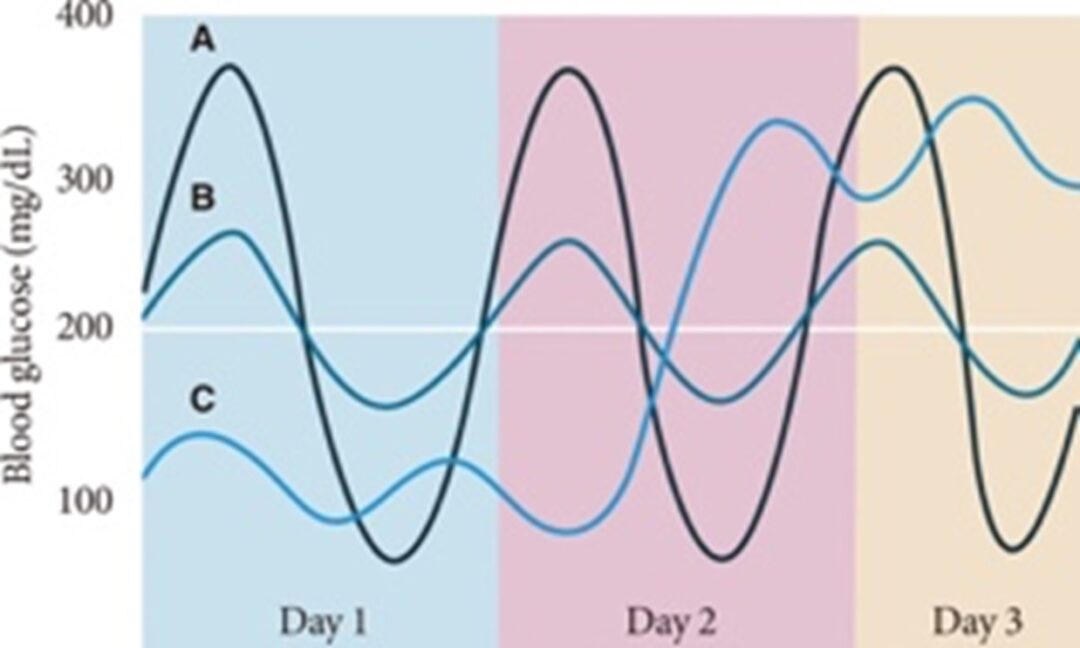 Image source: https://e-dmj.org/journal/view.php?doi=10.4093/dmj.2015.39.4.273
Image source: https://e-dmj.org/journal/view.php?doi=10.4093/dmj.2015.39.4.273
On the opposite end of this concept are blood sugar rollercoasters (picture posted above) that typically start with a post-meal blood glucose spike before scrambling to bring it back down, then up, before juggling to regain some blood sugar balance sooner rather than later.
This may also occur with blood sugar dropping too low to lead off this rollercoaster “ride.”
Something that may surprise you is that not only does carb quantity matter when it comes to blood glucose levels but so does its quality.
There are high glycemic foods capable of spiking up blood sugars almost immediately within 10 – 20 minutes of consumption.
There are also highly processed and refined foods that neither favor healthy insulin nor blood glucose levels.
I’m looking at you: fried foods, pizza, and mostly any other gluten-containing edible treat!
I’ve mentioned before that hyperpalatable (your taste buds love these) foods have a strong association with overeating, type 2 diabetes, and obesity (8, 9).
Again, these foods are typically high in carbs and require more insulin to accommodate them. In addition, you likely won’t stop after eating just one M&M or chocolate chip cookie.
However, 50 calories of pizza differ from 50 calories of broccoli or grilled sweet potato wedges.
If low-carb/high-protein, whole foods are your primary choice, it won’t likely take much to get you and keep you feeling full.
Whole foods are much higher in protein and fiber and lower in calories compared to the standard American diet (SAD).
All of this helps to make you feel full without any need or want to eat more than your body needs (10).
With the reduction of insulin demands, even if there is a miscalculated dose, the negative results are not typically as bad as with a larger and miscalculated insulin injection.
Overall, eating a whole-food, low-carb diet typically reduces:
- Insulin demand and blood glucose levels
- Overeating and frequent snacking
- Roller coaster blood sugar (glycemic variability) risk
- Obesity risk
Not too shabby, right?
But is there any medical proof that low-carb diets help blood sugars?
The Medical Research Behind the Low-Carb Benefits

A Harvard and Duke University study was performed on type 1 diabetic adults and children who followed a low-carb diet. The results showed an average A1C of 5.6%. This is equivalent to 114 mg/dL most commonly used in the United States or 6.3 mmol/L that is generally used everywhere else in the world (11).
A randomized clinical trial showed an average A1C of 6.16% (130.1 mg/dL; 7.2 mmol/L) reduced to a 5.93% (123.5 mg/dL; 6.9 mmol/L) range after six months on low-carb meals among prediabetics (12).
Another study saw insulin levels drop by as much as 150 units per day in 8 days, marking blood glucose improvements when reducing carb intake (13).
Not only that but there is even research supporting that the standard diet for blood sugar management has a low success rate among 18 different diabetes centers that care for approximately 8,000 type 1 diabetics (14).
What did they find?
The average A1C for this population was 8.2% (189 mg/dL; 10.5 mmol/L).
Compared to all the low-carb research just reviewed, this could look much better!
Low-Carb Flaws
 Gif source: https://tenor.com/bIftX.gif
Gif source: https://tenor.com/bIftX.gif
I’ve gone over quite a few physiological and diabetic benefits from eating a low-carb diet.
However, this doesn’t mean there aren’t a few hurdles to be aware of!
It May Be Difficult to Accept No Longer Eating Some (or Many) Foods Moving Forward
On paper, I’m sure all of this low-carb stuff sounds manageable enough to pursue successfully.
That is until…
…that work Christmas party or your kid’s friend’s birthday comes up. And the only foods provided are not part of this low-carb protocol.
What, then, do you do?
I believe the majority of type 1 diabetics who have no patience to try this low-carb regimen are likely not willing to accept this mandatory lifestyle change in diet.
I’ve heard multiple responses, such as:
- I have to have my pizza, though!
- I can’t give up on my pasta! Are you nuts?!
- But I love my soda!
Again, as long as your blood sugar results are what you want consistently, you keep doing what’s working.
But if your current BGs are not generally in the range you seek, these blood sugars will not likely change unless you’re sick and tired of being sick and tired.
Sometimes, if I know I’m going somewhere that will not cater to my dietary needs, I’ll stuff my face before leaving so that I’m so full; I have no desire to be tempted into eating anything I know won’t help my BGs.
I do the same for long travel days to avoid the most highly processed airport options.
Simply put: Without intention, optimal blood sugar management is a lost cause.
Missing in Action: Fiber

Dietary fiber is a carbohydrate that cannot be digested into glucose.
As a result, it is fermented by our gut microbes that turn them into short-chain fatty acids (SCFAs).
This fiber-to-SCFA transition typically feeds our gut bugs that have been shown to support (15, 16):
- Regular bowel movements
- Gut health
- Blood glucose levels
- Healthy body weight
- And more!
The Dietary Guidelines for Americans recommends a minimum of 14 grams of fiber per 1,000 calories consumed or up to 30 grams/day (17).
However, hunter-gatherer groups’ research has suggested revising this minimal standard.
How far off is this fiber intake recommendation?
To put things into perspective, it’s been shown that current hunter and gatherer groups eat approximately 100 – 150 grams of fiber/day from various plants and fruits currently in season (18).
Meanwhile, although it’s recommended we eat 30 g of fiber/day, much of society appears to be eating no more than 15 – 26 g/day (19, 16).
Now, if you add a low-carb diet into the mix, this daily fiber intake will likely drop even more, as many fiber-rich foods usually have more carbs.
A Type 1 Diabetic Needs Their Fiber & Fermentable Foods!
Though a low-carb diet may be tremendously advantageous for healthier and more sustainable blood glucose levels, unfortunately, it will typically be short on fiber.
The reason why is that many fiber-rich whole foods are also high in carbs.
This reduction in fiber will limit short-chain fatty acid production and its benefits in the body.
One way around this is to ask your doctor about supplementing with certain types of fibers that are typically low-carb..
A few fibers and fermentable foods to consider are:
- Resistant starch: cooked and cooled potatoes, jasmine rice, green plantains, yucca root; or prepackaged potato, green plantain, and green banana starch
- Fermentable vegetables
- Kefir
- Kombucha
- Psyllium husk
- Glucomannan
- Quality pre- and probiotics
I add in fermentable foods because these typically help to ensure a happy population of gut microbes exist.
I’ve also personally seen this make my diabetic management all the easier once addressing it.
A low-carb diet enriched with the right kind of dietary fibers can significantly contribute to healthier blood glucose levels.
Dietary fibers, particularly soluble fibers, play a key role in moderating blood glucose responses.
These fibers, found in foods like vegetables, fruits, and tubers, slow down the digestion and absorption of carbohydrates (20).
This results in a more gradual increase in blood glucose levels, rather than the sharp spikes that can occur after eating simple, refined, or heavily processed carbs.
Soluble fiber, in particular, forms a gel-like substance in the gut, which coats your digestive track and slows the breakdown of carbs and the absorption of sugar, helping to regulate blood sugar levels after your meals.
This is why it’s encouraged to consume fibers first thing and carbs last as this helps to reduce blood sugar spikes or the severity of them (21, 22).
For non-diabetics, this means that insulin is released more gradually, which is beneficial for insulin sensitivity.
For type 1 diabetics, this generally reinforces a less volatile blood sugar experience after meals, especially if a low-carb/high-protein diet are already being practiced..
Improved insulin sensitivity means the body’s cells are better able to respond to insulin, thus effectively managing blood glucose levels!
Moreover, a diet high in fiber can aid in weight loss and maintenance, which further contributes to improved blood glucose control.
Excess body weight, particularly around the abdomen, is associated with insulin resistance and higher blood sugar levels.
In summary, incorporating the right kind of fibers into a low-carb diet can help slow carbohydrate digestion, reduce blood sugar spikes, improve insulin sensitivity, and assist in weight management, all contributing to healthier blood glucose levels!
A Type 1 Diabetic Warning
Suppose you already have a gut condition, such as gut dysbiosis or small intestinal bacterial overgrowth (SIBO). In that case, the fiber you consume may worsen your current symptoms until these gut pathologies are treated and eliminated.
A common reason for this occurrence is due to these fibers feeding your gut microbes or gut bugs. If there are more bad gut bugs compared to the good ones, this is the most common reason why fibers and prebiotics can lead to the worsening of symptoms.
Which is just a red flag to get your gut addressed ASAP!
So, please keep this in mind.
Remember that almost everyone with an autoimmune condition likely already has some form of gut dysbiosis that can be detected well before their autoimmunity has been officially diagnosed (22).
I hope this information was insightful and educating. If you feel this would help to empower another individual with a blood sugar disorders, please share this with them and thank you!
Summary
- Some benefits a type 1 diabetic may have in eating a low-carb diet may be:
- Reduced insulin demand and cost
- Lower blood sugars with more consistency
- Increased insulin sensitivity
- Longer range of healthy blood glucose levels
- Decreased rollercoaster blood sugars
- Medical research supports a low-carb diet in better managing blood sugars
- 2 Important Factors to Note When Starting a Low-Carb Diet for Blood Sugar Benefits
-
- Unless you’re sick and tired of being sick and tired or extremely well-disciplined, it may be difficult to stop eating non-helpful foods (that may also be your favorite treats)
- A low-carb diet typically encourages a reduced intake of fiber, which has many health and blood sugar benefits
- Ask your doctor about supplementing with some of the fibers I mentioned
- Be warned that if you already have gut dysfunction, increased fiber intake may worsen your symptoms or cause flair ups
References
2. https://www.amazon.com/Dr-Bernsteins-Diabetes-Solution-audiobook/dp/B01N74YJUG/ref=sr_1_4
3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4512569/
4. https://www.umassmed.edu/dcoe/news/umass-diabetes-news/2018/may/low-carb-diet-t1d/
5. https://diabetesjournals.org/care/article/31/Supplement_2/ S262/24841/Insulin-Resistance-and-HyperinsulinemiaIs
6. https://pubmed.ncbi.nlm.nih.gov/29939616/
7. https://www.lilly.com/resources/insulin-affordability
8. https://www.diabetes.co.uk/news/2023/feb/hyper-palatable-foods-increase-your-calorie-intake-study-shows.html
9. https://www.omicsonline.org/open-access-pdfs/type-2-diabetes-has-a-high-correlation-with-food-addiction.pdf
10. https://www.sciencedirect.com/science/article/pii/S0924224414002386
11. https://publications.aap.org/pediatrics/article-abstract/141/6/e20173349/37619/Management-of-Type-1-Diabetes-With-a-Very-Low
12. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2797714
13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2315645/
14. https://pubmed.ncbi.nlm.nih.gov/34142758/
15. https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/fiber/art-20043983
16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9787832/
17. https://diabetes.org/healthy-living/recipes-nutrition/understanding-carbs/get-to-know-carbs
18. https://www.science.org/doi/10.1126/science.aan4834
19. https://www.ucsfhealth.org/education/increasing-fiber-intake
20. https://www.cdc.gov/diabetes/library/features/role-of-fiber.html
21. https://pubmed.ncbi.nlm.nih.gov/30381620/
22. https://pubmed.ncbi.nlm.nih.gov/36904173/
23. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6854958/


